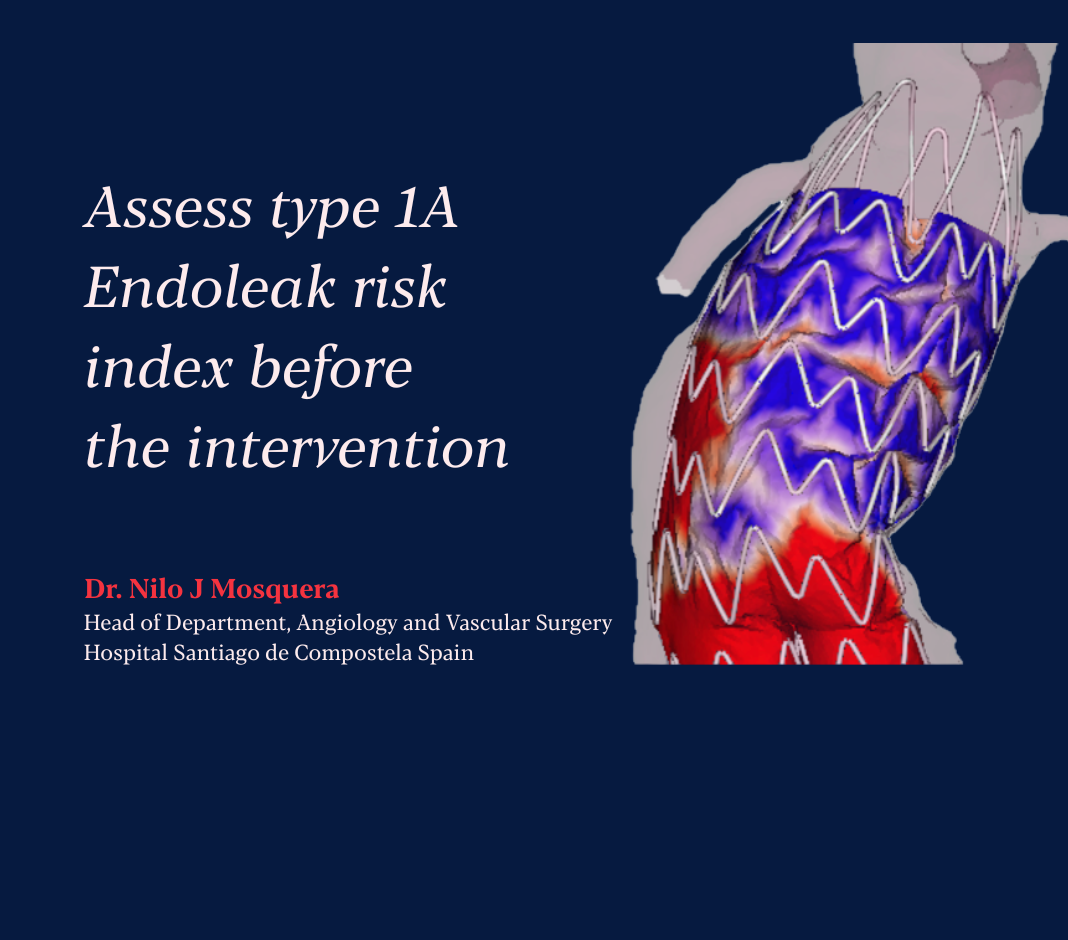
Endoleak Risk Index (ERI)
Guiding surgeons toward optimal device selection to reduce the chances of complications and enhance patients’ outcomes.

Assess type 1A Endoleak risk before EVAR intervention
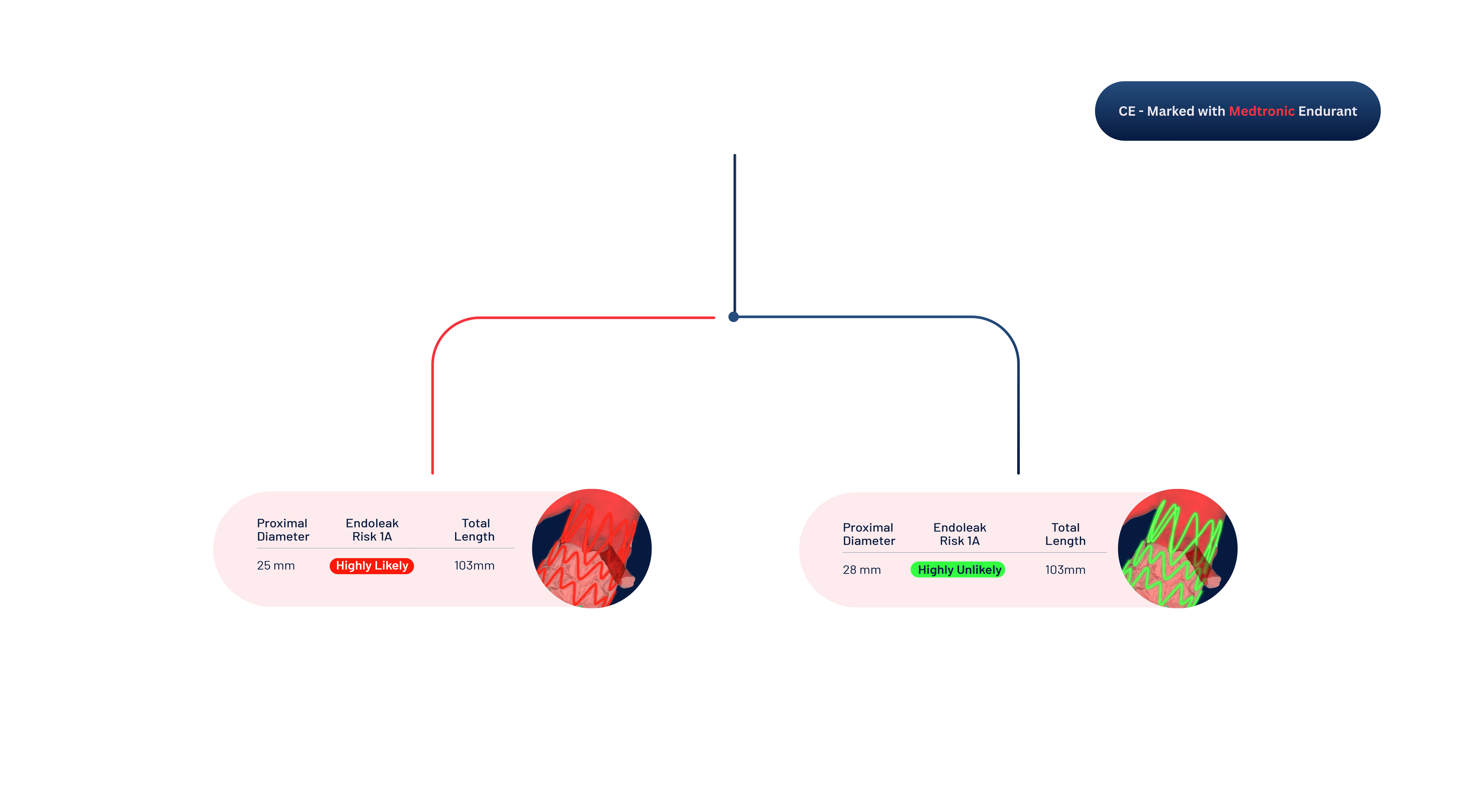
Explore various endograft diameters, landing zones and choose the optimal configuration for the patient
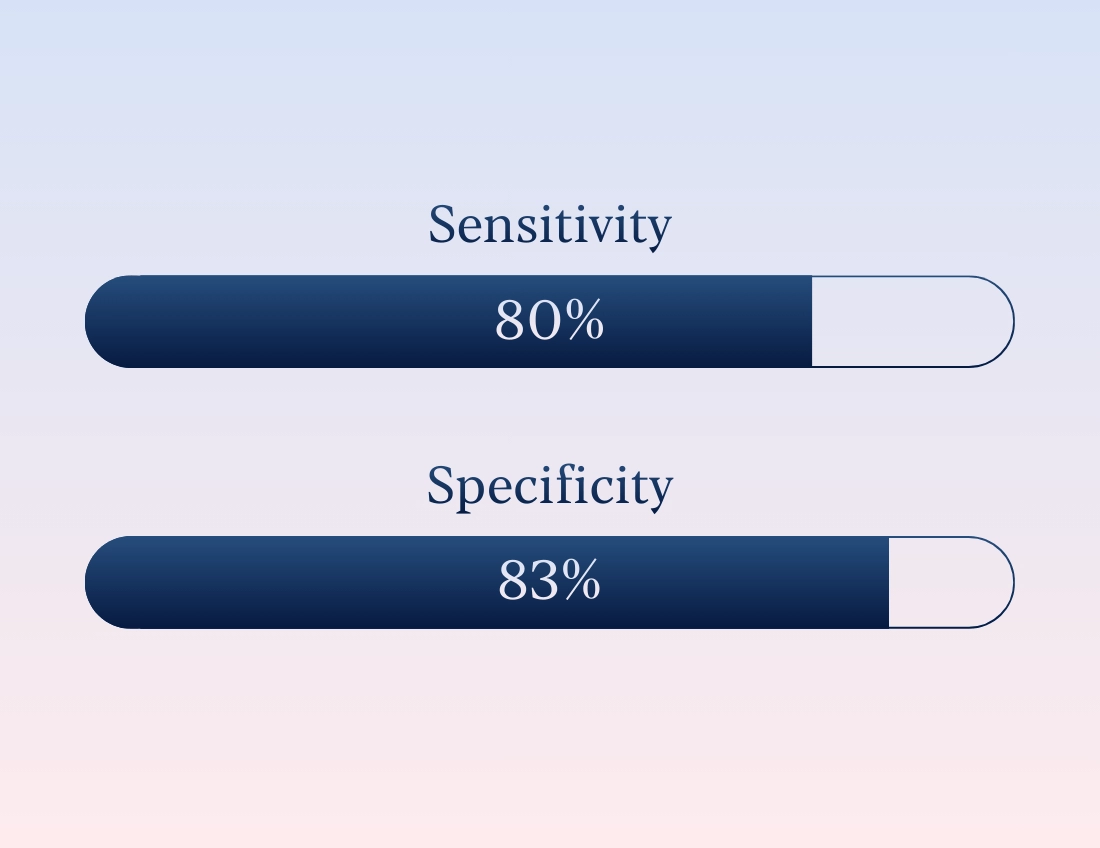
Clinical Validation
Validation Study - EnduSim II
Retrospective European multicenter study - ongoing enrollment: Prof Antoine Millon, University Hospitals of Lyon.
Training dataset: 117 patients (Type 1A endoleaks: 34 (13 early, 21 late), 83 controls.
Validation dataset: 56 patients Assessment blinded to Endoleak status. 20 type 1A Endoleaks (6 early, 14 late), 36 controls.
AI-Powered EVAR Planning
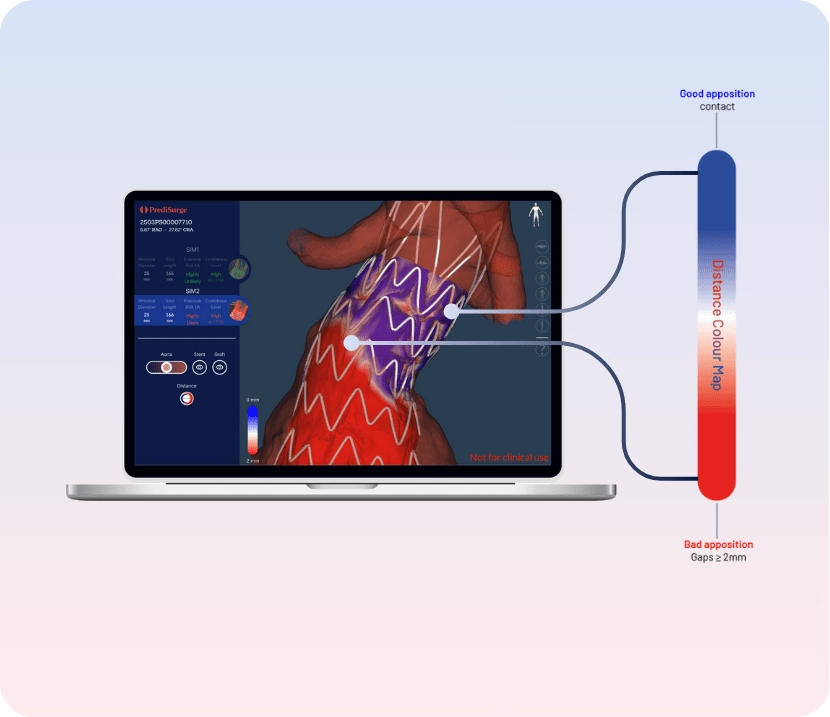
Distance Colour Map
With iView Colour, instantly highlight the apposition gaps between the graft and aortic wall thanks to Distance Colour Map.
The expert perspective
First-hand experience from operating rooms to R&D labs — professionals trust PrediSurge to improve outcomes, enhance safety, and accelerate innovation.
Clinical Stories
Insights from clinical and R&D practice, directly from our experts
Press highlights & Insights
Independent recognition through clinical research and media coverage and PrediSurge insights
Frequently asked questions
What is aortic digital twin?
From a patient’s pre-operative CT scan, the aortic digital twin is created to faithfully reproduce both the shape and the bio mechanical behavior of the real aorta. This advanced 3D model allows precise simulation of how the patient’s anatomy responds to mechanical forces, providing a reliable virtual counterpart of the vessel.
What is ERI?
ERI stands for Endoleak Risk Index, is an AI-powered index based on the analysis of the intervention simulation, with a specific focus on the proximal apposition between the endograft and the patient-specific aortic digital twin. It assesses preoperatively the risk of Type IA endoleak associated with EVAR.
How is ERI calculated?
Each EVAR simulation automatically analyses the proximal aortic neck using 40 cross-sectional slices. For each slice, the aortic wall and endograft are sampled at 200 points each to measure local radii and apposition. This generates up to 16,000 detailed measurements per patient.
Are thrombus and calcifications taken into account?
It is important to distinguish between two different stages of analysis:
- Simulation: Only the aortic lumen is modeled; thrombus and calcifications are not yet included.
- Risk assessment (ERI): Thrombus burden is included as a variable in the machine-learning model used to compute risk.


.webp)